Editors Note: This article first appeared on The War Horse, an award-winning nonprofit news organization educating the public on military service. Subscribe to their newsletter.
Jen Burch served a seven-month tour in Afghanistan a decade ago.
It has haunted her ever since.
Burch, who was 23 when her tour ended, worked as an operations manager for an Air Force combat engineer unit. She aspired to be a physician. She spent her downtime as a volunteer medic at a Kandahar trauma hospital.
“I saw the worst of war and the best of humanity,” she says.
She came home with the service’s prestigious Commendation Medal, awarded for acts of valor or meritorious service. She also brought home a case of post-traumatic stress, frequent migraine headaches, and bronchitis and other breathing problems. But help has been slow in coming — both for Burch and for other veterans, she says.
“They need peer community support and easier access to health care and benefits,” says the 34-year-old retired Air Force staff sergeant. “Everything moves at this bureaucratic pace.”
While many Americans may have seen the end of the forever wars as the cap on two decades’ worth of war spending, the job of Veterans Affairs has only just begun — and will continue for decades. But some fear the antagonistic relationship between VA and veterans will continue as advocates are forced to fight bureaucracy to gain benefits, even as VA officials say they’re ready to move forward.
“As we look to the future, we’re not trying to build a VA that goes back to the old normal,” VA Secretary Denis McDonough recently said at the National Press Club. “Instead, we’re going to continue to do better for vets, we’re going to continue to be better for vets.”
While VA projects the numbers of veterans will decline — from 20.8 million in 2015 to 12 million in 2045 — VA spent almost $218 million on veterans in fiscal year 2020. That’s nearly double what it spent in fiscal year 2010. The benefits go far beyond health care and disability benefits: Veterans can get help buying their first homes, money for college, and even end-of-life benefits like a burial plot.

But veterans and their advocates say they have immediate needs, life-or-death needs, that must be met as two decades’ worth of battles end. They want presumption for the harmful chemicals and particulate matter they were exposed to both in war and at home. They want better mental health care. They want their friends to stop killing themselves. They want a truly seamless transition from active duty to VA. And they want better treatments.
They want those things for yesterday’s veterans, too.
‘The issues are clear’
Health concerns like PTSD and toxic exposures are not new. But the veterans’ community, including VA and its allies in Congress, needs to redouble its efforts, supporters said.
“The issues are clear,” says former VA Secretary David Shulkin. “In hospitals, we need more centers of excellence on issues that impact veterans and more open approaches to new treatments. We need updated payment systems and technology for VA in order to better fulfill its mission.”
With almost 400,000 employees, VA is a sprawling government agency that manages everything from hospitals where cutting-edge medical technology restores bodies broken by the savagery of combat, to the cemeteries where so many veterans find their final rest.
It is seen as both a source of empathetic outreach and support to those who have worn the uniform and their families, and a vast, cold bureaucracy more concerned with costs than its mission.
“I don’t believe there is anyone at VA that is malicious and tries to harm veterans,” said Michael Figlioli, deputy director of the Veterans of Foreign Wars’ National Veterans Service. “It’s such a big bureaucracy. It just takes a long time to get things done.”
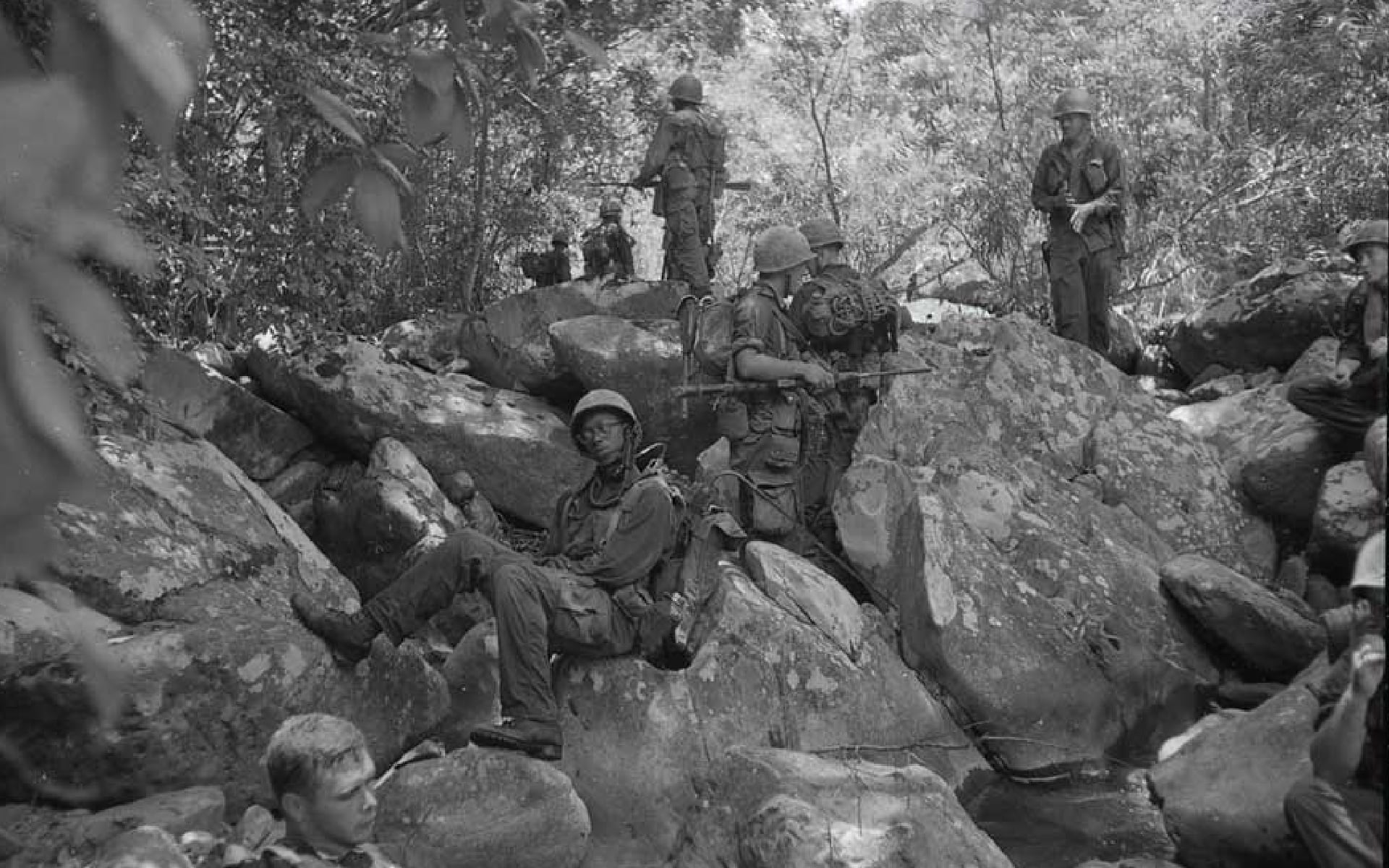
Looking to previous wars — Vietnam, Desert Storm, even World War II — doesn’t leave veterans hopeful. It took years before VA began to recognize that exposure to Agent Orange was harmful. The compound was a chemical defoliant used during the Vietnam War to eradicate the jungle cover used by the Viet Cong. Exposure led to cancers and other health problems among U.S. troops.
It’s been the same story with Gulf War illness, a chronic disorder with multiple medical symptoms experienced by troops who served in Iraq. They have battled VA since the 1990s over its deleterious impact on their health.
And World War II veterans fought for benefits after being exposed to radiation in Hiroshima and Nagasaki, Japan, after the atomic bombs, as well as because of exposure during nuclear tests conducted by the United States. They did not receive benefits until 1996.
Much of the problem comes from bureaucracy — paperwork and backlogs and appeals.
Figlioli told an investigations subcommittee of the House Committee on Veterans Affairs in July that VA insists on requiring veterans with Gulf War illness claims to fill out a Disability Benefits Questionnaire for every symptom they experience. It only considers Gulf War illness to be the cause of their condition “as a last resort,” he said.
Instead, VA should just decide that the medical evidence meets the criteria.
“The current system of assigning separate [Disability Benefits Questionnaires] for each symptom being claimed in association with GWI [Gulf War illness] promotes the potential for incorrectly assigning a diagnosis to a condition linked to GWI … which ultimately results in the veteran’s claim being denied,” Figlioli told the subcommittee.
But much of it also comes from the sense of an antagonistic relationship between veterans and VA employees — that the hurdles veterans face are intentional.
Shulkin, a physician, said “bad policy” causes the disability claims of so many veterans dealing with toxic exposures to be turned down.
‘We’re not waiting for Congress’
But with the withdrawal from Afghanistan and new leadership at VA that might be more receptive to their concerns than the previous administrations, veterans, their advocates, the organizations that lobby for them, and other allies all say that toxic exposure is one of the top issues that demand immediate attention.
“How many people need to die,” Burch says, “before they figure out they need to get something done?”
She had been stationed in the sandy deserts in southern Afghanistan where toxic particles in the thick black smoke from the burn pits mingled with the dust and permeated the air she breathed.

She had hoped to stay in the Air Force and eventually become an officer. But her health began to deteriorate, and she medically retired in 2014. She was in and out of emergency rooms and hospital beds for several years because of migraines and pulmonary problems.
Now she uses an inhaler.
“Before Afghanistan, I was an avid runner,” she says. “I came home barely able to run a mile without stopping to cough.”
The burn pits have been linked to a variety of serious ailments among veterans who were deployed to the Middle East and Southwest Asia, including cancer and respiratory problems. Yet between 2013 and 2020, VA denied 78 percent of the disability claims related to toxic exposures, according to department data.
“It’s the modern-day Agent Orange,” Burch says. “There are a lot of veterans suffering, who are coming down with cancers and all sorts of health conditions.”
But the Biden administration says it is paying attention — and making changes. Recently, VA gave presumptive status to asthma, rhinitis, and sinusitis for all veterans who served in Southwest Asia since 1990 — as well as in Afghanistan, Djibouti, Syria, and Uzbekistan during the Persian Gulf War or since Sept. 19, 2001.
Burch, however, says she is impatient with the White House plan to have VA do a 90-day review of rare forms of cancers that might qualify for service connection.

“We have all this information,” she says. “We don’t need to take another 90 days. There are people who don’t have 90 days. It keeps getting pushed back. It’s like, c’mon. Cut the bureaucracy and get this done.”
McDonough says they’re updating the system they use to determine which conditions should be presumptive more quickly, and that, “for the first time in VA history,” they’re “presumptively paying toxic exposure claims” to Gulf War veterans for several conditions.
McDonough acknowledged the new presumptions have led to a backlog — but said VA had hired 2,000 people to help push through those claims.
“Veterans have waited far too long for those benefits,” he says, “and we’re doing everything in our power to make sure they won’t have to wait any longer.”
As evidence, VA spokesman Randal Noller says the 78 percent denial rate for burn pit exposures is no longer accurate because the department no longer asks veterans to specify “burn pits” in their disability claims.
“In Iraq, Afghanistan, and Djibouti on the Horn of Africa, from approximately 2001 to the present, the U.S. military has used large burn pits to dispose of waste at every location wherein the military has positioned a forward operating base [FOB],” Noller said in an email. “Therefore, if a veteran was deployed to one of these locations or elsewhere in Southwest Asia, VA will concede exposure to burn pits.”
From Agent Orange to Gulf War illness to burn pits, veterans and their advocates have battled VA for decades over the medical legitimacy of their claims that their health problems are the result of their military service. Presumption means veterans receive VA health care and benefits because of that connection.

But there’s been a change in tone.
VA recently changed its website language about burn pits from “no known connection” to, “Depending on a variety of factors, you may experience health effects related to this exposure.”
“We’ve already processed more than 3,800 claims, delivering millions of dollars in benefits that vets so rightly deserve,” McDonough said about burn pit claims while talking with reporters in October. “We’re not going to wait for Congress to act on this. We’re acting ourselves and we’ll have more news on that front.”
“More news” referred to a fact sheet released by the White House on Veterans Day that, among other things, highlighted efforts to let veterans know they have been exposed, train all health care workers about toxic exposures so they can better treat veterans, set up a toxin-specific call center, and ask Congress to extend recent veterans’ free VA health care program for veterans who deployed to Iraq or Afghanistan.
On Capitol Hill, several bills are in the works that would make toxic exposure eligible for presumptive care: If former troops can show service near where burn pits were in operation and suffer from the kinds of illness associated with them, they would automatically qualify for VA treatment and disability benefits.
“Providing health care and benefits to veterans suffering from the effects of toxic exposure is a cost of war that must be paid, and it’s well past-time for Congress to deliver on this promise,” Sen. Jon Tester, D-Montana, said in an email. “Veterans simply can’t rely on piecemeal legislation any longer, and this legislative package is our best shot at ensuring past, present, and future generations get their due health care and disability benefits.”
‘I have concluded it’s faster than me’
Advocates also want more programs to help veterans suffering from post-traumatic stress and other mental health problems brought on by their military service.
“This is something we see everyone struggling with,” said Kelly Hruska, government relations director at the National Military Family Association. “For the military, especially transitioning military, there is an acute need.”
Jason Kander knows all too well what many veterans are going through and how, without a concerted outreach effort, they can become adrift and tormented by their memories.
Kander was an Army intelligence officer in Iraq in 2006. It was a job that put him “with no backup … outside the wire meeting with people of questionable allegiance, not knowing whether you’d be able to get out of the room alive,” he tells The War Horse.
His work took a toll on his mental health. But he refused to acknowledge it and tried to paper over his anxieties with public service. After he came home, he catapulted to political prominence.
A liberal Democrat in a conservative red state, he did stints in the Missouri Legislature and as secretary of state before running for the U.S. Senate in 2016 and nearly toppling a powerful Republican, Sen. Roy Blunt.
Suddenly, Kander became an up-and-coming political star. In 2018, he was considered the frontrunner in the race for Kansas City mayor when he suddenly folded his campaign. He said he needed to finally deal with the mental health issues that had been plaguing him since he left Iraq.

“So after 11 years of trying to outrun depression and PTSD symptoms, I have finally concluded that it’s faster than me,” Kander announced at the time. “That I have to stop running, turn around, and confront it.”
He now serves as president of the Veterans Community Project, which addresses health care, poverty, homelessness, and other concerns in veterans.
In an interview, Kander says one of the difficulties in getting veterans with PTSD to seek help is that so many of the portrayals on TV and in movies end tragically.
“What I think of as ‘PTSD porn,’” he said. “It keeps people from getting help. If you get diagnosed with PTSD, it’s the end of the story. It’s not.”
Burch’s dreams also changed because of PTSD. When she left the service, Burch switched from pre-med to public health. But just being inside a hospital awakened her memories of the damage and the devastated lives she saw while working in the Kandahar hospital.
“Anytime I would do shadow in the ER, I started to have a lot of flashbacks,” she says. “I was feeling like I was reliving a lot of it. I started having cold sweats.”
Burch changed her professional goals. She accepted a position at Iraq and Afghanistan Veterans of America in December after serving as a senior military fellow there since September.
‘It’s a crisis’
The huge number of veterans killing themselves also concerns the advocates. They kill themselves at a rate 1.5 times greater than civilians do, with post-9/11 veterans killing themselves at a rate of 2.5 that of civilians the same age — and service members are screened for mental health issues before they join the military. More than 17 veterans took their lives every day in 2019, according to VA’s latest report. More than half had never had any contact with VA’s Veterans Health Administration.
Military Times reported in August that calls to VA’s Veterans Crisis Line spiked around the time the U.S. pulled out of Afghanistan.

“It’s a crisis,” says Tom Porter, who heads the Washington office of Iraq and Afghanistan Veterans of America.
A new law, sponsored by Tester and Sen. Jerry Moran, R-Kansas, and signed into law in October of 2020, allows VA to hire more mental health care workers, adds suicide prevention coordinators to VA hospitals, holds VA accountable for suicide prevention programs, and ensures veterans in rural areas have access to suicide prevention resources.
Advocates say some of these needs could be addressed with one seemingly simple measure: automatic enrollment into VA as soon as troops leave the military so they can immediately access health care if they need it. It serves as a gateway to a variety of other VA services, including home loans, the G.I. Bill, insurance, programs for women, and more.
“It’s super important,” Kander says. “You get out of the service on Tuesday. Monday, your government knew everything that was going on with you. Tuesday, you show up at the VA. It’s like they, like, never heard of you.”
This War Horse feature was reported by David Goldstein, edited by Kelly Kennedy, fact-checked by Ben Kalin, and copy-edited by Mitchell Hansen-Dewar.
David Goldstein is a freelance journalist in Washington who has covered government and national politics, including several presidential campaigns, for more than two decades. During stints with McClatchy Newspapers, Knight Ridder, and The Kansas City Star, he has written about the pre- and post-deployment health problems of troops deployed during the Iraq War, their struggles with Veterans Affairs, and the toxic exposure of veterans involved in Cold War chemical experiments.



